The start of the year can feel like a race — lists of goals, expectations, and pressure to “get it all done.” But real transformation comes when you pause and reflect: How am I doing with my goals? Am I at peace knowing I don’t have to do everything at once? Am I giving myself grace?
Many people set goals in January but feel guilt, frustration, or even shame if they aren’t “perfect” by February. The truth is: no one achieves everything at once. Growth is a journey, not a sprint.
Imagine you’re learning a new language. You wouldn’t expect to speak fluently in a week — you’d celebrate each new word, each small conversation. Your wellness journey works the same way.
Ways to Give Yourself Grace:
-
Pause and Reflect: Ask yourself, “What’s one thing I’m proud of since the year started?”
-
Release Perfection: Understand that slow, steady progress is still progress.
-
Adjust, Don’t Abandon: If a goal feels too heavy, scale it back instead of giving up.
-
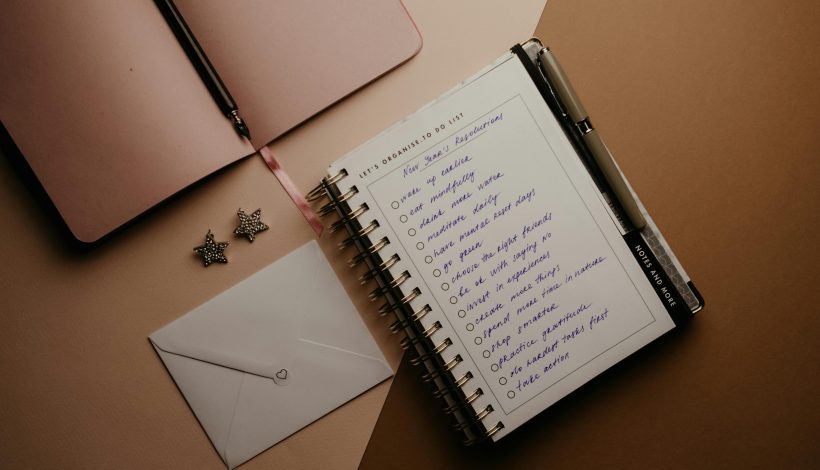
Celebrate Small Wins: Write them down — they’re proof of your commitment.
-
Focus on Peace: Your worth isn’t tied to productivity. Feeling calm and aligned is just as valuable as checking off a task.
Tip:
This year, give yourself permission to grow at your own pace. Reflect with kindness, acknowledge your wins, and allow space for peace. You don’t have to do everything at once — you’re allowed to be a work in progress.
This week, take five minutes to reflect on your goals. Write down one small win and one way you can give yourself grace moving forward.
Written by Rosie Moore, DNP, RN, LNC, BC-FMP