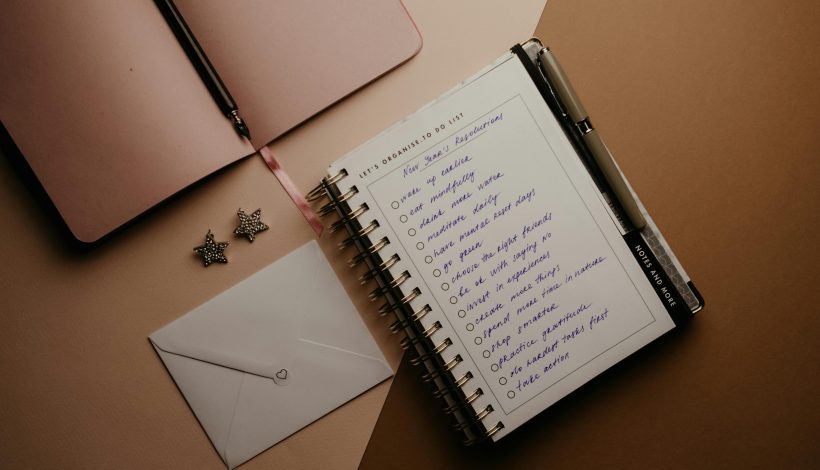
The New Year often brings hope, motivation, and a list of resolutions. But for many, this excitement quickly turns to frustration when goals feel overwhelming or unrealistic. Functional medicine and wellness aren’t about overnight change — lasting results come from pacing yourself and meeting yourself where you are.
Many people fall into the trap of:
-
Setting large goals that aren’t realistic for their current lifestyle
-
Expecting instant results and feeling discouraged when progress is slow
-
Comparing themselves to others who seem “perfect” or more disciplined
Think of it like planting a garden. You can’t expect a seed to become a full bloom overnight. You need water, sunlight, and care over time. Health goals work the same way — small, consistent actions compound into real change.
Tips for Achievable New Year Goals:
-
Start small: Pick one or two meaningful goals instead of a long list.
-
Focus on habits, not outcomes: Instead of “lose 20 pounds,” try “walk 20 minutes daily” or “add a vegetable to every meal.”
-
Celebrate small wins: Each completed habit builds momentum and confidence.
-
Be flexible: Life happens. Adjust your plan rather than giving up.
-
Reflect regularly: Check in weekly or monthly to assess what’s working and what isn’t — without judgment.
The key to New Year success isn’t perfection — it’s patience, persistence, and self-compassion. By pacing yourself and focusing on realistic, actionable steps, you’ll create habits that last well beyond January.
This week, choose one health or wellness goal and break it into small steps you can realistically take. Track your progress and celebrate each step forward.
Written by Rosie Moore, DNP, RN, LNC, BC-FMP