Your gut plays a central role in overall health, affecting digestion, immunity, and even mood. A balanced gut microbiome — the community of bacteria living in your intestines — helps protect against inflammation and supports proper nutrient absorption. Choosing the right foods can help your body cultivate beneficial gut bacteria naturally while reducing inflammation
Fermented foods are among the most powerful allies for gut health. Yogurt, kefir, sauerkraut, kimchi, miso, and kombucha contain live probiotics that help balance intestinal bacteria. These foods can improve digestion, reduce bloating, and enhance immune function. Even small daily servings can make a noticeable difference over time.
Prebiotic foods feed your beneficial gut bacteria, helping them thrive. Garlic, onions, leeks, asparagus, bananas, and whole grains are rich in prebiotic fibers that fuel probiotic activity. Pairing prebiotics with probiotic foods — for example, adding garlic to a sauerkraut dish — can maximize gut support and enhance anti-inflammatory effects.
Fiber-rich fruits, vegetables, nuts, and seeds also play a key role in gut health. They promote regular bowel movements, stabilize blood sugar, and reduce chronic inflammation that contributes to fatigue, joint pain, and cardiovascular risk. Eating a colorful variety ensures you get a broad spectrum of nutrients and phytonutrients to nourish your microbiome.
Patient Perspective:
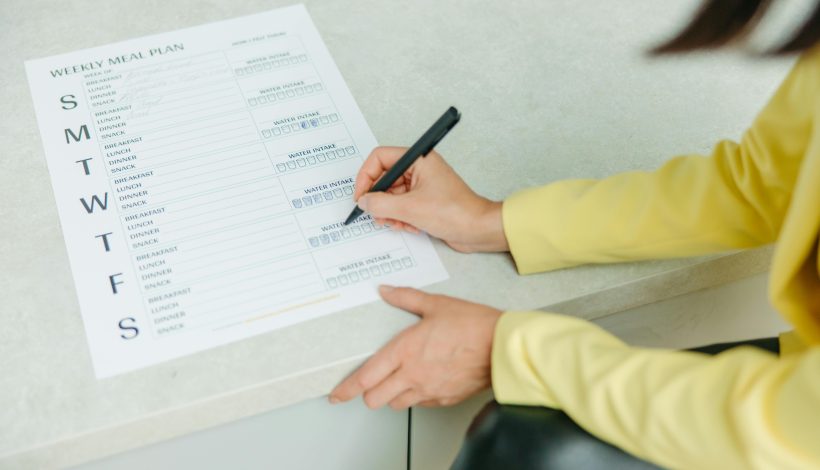
Improving gut health doesn’t require drastic changes. Introducing one probiotic-rich food and one prebiotic food per day is a simple start. Tracking how your body responds — such as reduced bloating, improved digestion, or better energy — helps reinforce habits and encourages long-term consistency.
Nursing Perspective:
Nurses support patients in understanding the connection between diet, gut health, and inflammation. Educating on probiotic and prebiotic sources, providing practical meal suggestions, and monitoring improvements ensures safe, sustainable lifestyle changes. Small, consistent adjustments can yield meaningful benefits for both gut function and overall wellness.
💡 Tip to Try This Week:
Add one fermented food and one prebiotic-rich food to your daily meals. For example, top your salad with a spoonful of sauerkraut and include a banana with breakfast. These simple choices support beneficial gut bacteria, reduce inflammation, and enhance digestion naturally.Written by Rosie Moore, DNP, RN, LNC, BC-FMP