An emergency room nurse asks how can he make changes in his emergency room to better serve the patients?
My response to the ER nurse was to acknowledge that I understood his enthusiasm in wanting to make the changes in his emergency department. In such a fast paced department where it is a matter of life and death, it is hard to implement changes because the nurses may feel they do not have the time to learn but as managers we know that a change must take place (Stevens & Caldwell, 2012). The emergency department is one of those places where there is never a happy medium making it difficult to staff and do trainings. But as the website for the American Academy of Healthcare Communication noted “communication is the key to exceptional patient care” (http://www.health.gov/communication/resources/Default.asp).
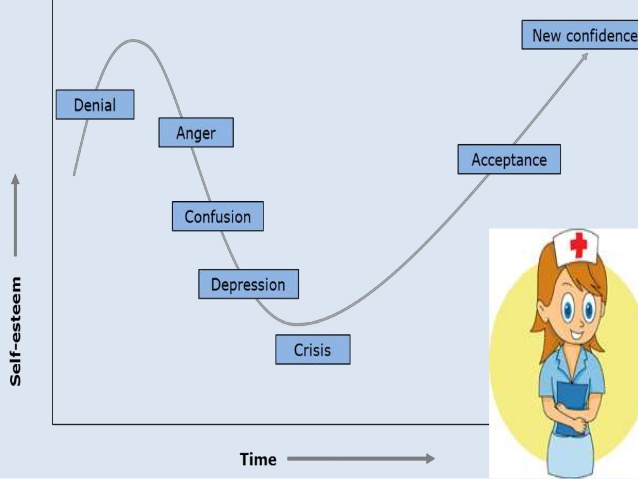
In order for the nurse to feel that there needs to be a change, there has to be an explanation to them impressing that remaining in the same pattern is not helping the patients. As managers though, we need to be careful on how this is communicated to the staff, because people are sensitive and if they feel that the work they are doing at the moment is not good enough, they will not accept new changes favorably.
One way to implement change is by communication in a narrative format; doing a synopsis of what has been happening in the emergency department. For example, how many patients have had complications as a result of starting an IV on patients with difficult vascular access because too much time was spent on trying to get an IV line in or calling someone else when attempts have failed? Without laying blame on anyone, if this study is brought as a statistic and narrative then it may help the nurses see the importance of a quick ultrasound to see the access.
Everyone is always afraid of change but if presented in such a format where they are given the time to learn it, for example paid education to come to the training on an off day with different options given for the training based on the two or three shifts that the hospital has. Once the plan is implemented for training, being able to have the educators follow-up with each nurse on how they are doing, will show the staff that the management genuinely cares. It is important to know if the new transition towards the change is working and if not why, so that the training can be revamped.
Once the nurses see that the change is going to make their jobs easier and the patient’s quality of care rises to a new level, they will be more receptive.
References
Stevens, K. R., & Caldwell, E. (2012, August 29, 2012). Nurse Leader Resistance Perceived as a Barrier to High-Quality, Evidence-Based Patient Care. The Ohio State University Research and Innovation Communications. Retrieved from http://www.health.gov/communication/resources/Default.asp