In every organization there are communication barriers, but overcoming them is part of being professional and respectful of others’ opinion. In some organizations the leadership structure has a medical director, senior health service director, a health service director, a manager and the case manager. The case manager manages the file, develops the plan of care with the assistance of the member or the family. The nurse is responsible to ensure that the member is attending their doctor’s appointments, taking their medications and maintaining their insurance eligibility monthly. This should be done by the social worker however in some organizations, the social workers manage the same types of patients that the nurses manage.
There are other professionals on the team that help maintain the members with their eligibility for their Medicaid insurance. Part of the team is the operations team. This is where things in an organization get blurred due to communication gaps, lack of resources, support and professionalism. The team in operations are not nurses. The operations team will email the nurse and copy the manager to let them know that the member is going to lose eligibility if they do not send in their paperwork timely to the state. When the nurse receives this email, the nurse is to drop all that they are doing to attend to the member’s eligibility. This will involve contacting the state to see what is happening with their eligibility. This is something operations can handle but they state their function is just to advise the case managers of the discrepancy.

Another barrier that is seen in management of cases is the inability to show respect to other team members and allow a learning environment. One agency case manager stated that every two weeks the team of case managers reviews case files on a conference call with the medical director. These cases are reviewed in their team meetings weekly before submitting to the medical director and as a team they discuss what has been done and make suggestions. The cases are emailed to the medical director and his assistant selects the cases. Recently, a case manager stated that two cases were selected for review from her team. The case managers present them to about one hundred and eighty people or more on the call from directors to managers and case managers. As the doctor asks his questions and makes his recommendations, the case manager indicated that her director, who is her manager’s superior, made a statement on both cases stating to the team that their manager should have known this and taken a different approach before sending this to review. The case manager did not know what to say, but this was stated over and over about five or six times throughout the presentation of both cases. At the end, what was stated by that director was if your manager does not know what to do, then call her. This is a prime example of a barrier in trying to be in a learning environment that will help the case manager grow and benefit the patient. (Rubenfeld & Schaeffer, 2014)

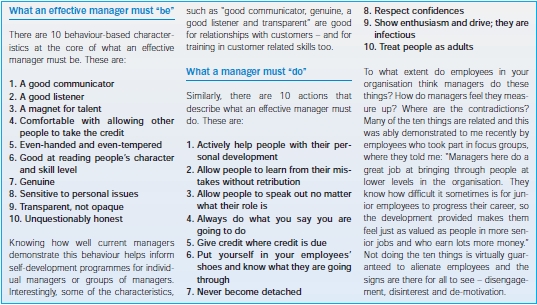
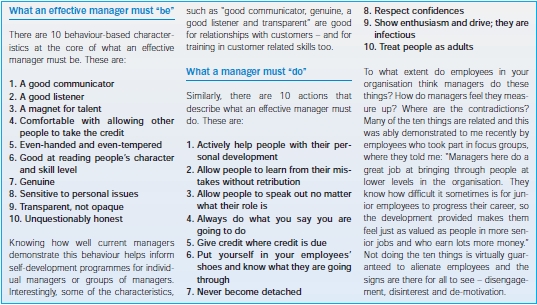
Collaboration can only exist in a team when the leader uses critical thinking, an interdisciplinary team approach and collaborate on cases together. But in the big picture of corporate America under some managers this is not acceptable, it is more along the lines of a multidisciplinary team. In this type of team, you only have individual thinking in the group, meaning their way and no other opinions. The focus will be on tasks and check off systems regardless if it is feasible to do. (Rubenfeld & Schaeffer, 2014)

In conclusion, nurses do have the ability to be leaders, educators and changers of a system, if assertive enough to make that change, but in order to do so a good team of interprofessional people are needed. Because at the end of the day, the patient is who counts and why changes are necessary.
References
Rubenfeld, M. G., & Scheffer, B. (2014). Critical Thinking Tactics for Nursing Achieving the IOM Competencies (3rd ed.). [P2BS-11]. Retrieved from http://online.vitalsource.com/books/9781284059571
Written by Rosie Moore, RN, BSN, LNC