How Nursing Has Evolved Through the Years
Nursing has evolved throughout the years thank goodness to a different level of respect. Although I do believe that some doctors and even nurses still carry the old way of practicing where the doctor is the lead and nothing else matters. This is I believe even differs from the North to the South. I remember graduating from nursing school and working with the doctors in labor and delivery who are now looking at me not as the kid in school, but as the professional on their team. The doctors would say call me Mike, or John when we were not around the patients and it was a comfortable working relationship (not to the extent of the TV show dramas, that is not realistic!) making everyone’s job easier, especially for a new grad that had questions.
When I moved to Florida I noticed that the nurses and staff would say Dr. Smith or Dr. Jones and he would say whatever it is he needed and the nurse would say yes sir, is there anything else that I can do for you. It was the politeness of the South or the servant of the South one or the other. I thought to myself, okay this is certainly going to take some getting used to if I am going to live in Florida. In no time at all, I had to conform since I wanted to be gainfully employed.
When I think of being on an interprofessional team, I think of the team that I was in up North, where it was a comfortable open ended relationship between nurses and doctors to discuss what was happening with the patient and come up with a plan. When I think of being on the interprofessioal team in Florida when I first moved here, that to me was not a team. It was a nurse and a doctor, with the doctor stating what needed to be done, the nurse saying yes sir and doing what she was asked. It should be a partnership collaborating together (Sommerfeldt, 2013).
Many years have evolved since I first moved to Florida and I have seen the change happen where nurses can have a more involved relationship with doctors as a team player and include nutritionists, therapists and discharge planners. There are still some rigid single minded doctors out there that will not work on an interprofessional team; however our job is not to change them. We can spend a long time trying to make changes and getting our point of views heard, but if we can make an impact with what we can control in our scope of practice, this will go a long way to improving healthcare.

Sommerfeldt, S. C. (2013, February 25 2013). Articulating Nursing in an Interpersonal World. Nurse Education in Practice, (13), 519. http://dx.doi.org/http://dx.doi.org/10.1016/j.nepr.2013.02.014
Follow Rosie Moore https://www.facebook.com/rosiesnursecorner/
The Nurse Leader of a Healthcare Team
A nurse can play three different roles as part of an interprofessional team. The three roles consist of a nurse, nurse leader and nurse educator. The interprofessionalism team consists of other healthcare workers as well, not just nurses (Sommerfeldt, 2013). However as nurses the roles can be at different levels depending on the patient’s condition. At my previous job, I worked as a complex case manager. The team consisted of registered nurses, social workers (masters prepared) behavioral health specialists, community health workers and nutritionists. The nurse case manager managed the patient, however if there was an issue with the patient in the home setting that required community resources, the community health worker would be consulted to assist in those needs. If the member had psychological issue or other financial issues that required the need of a social worker or behavioral health specialist this referral would be added as well. There was collaboration on the plan of care and all participated because we all were looking at the patient as a whole, not just as the part that each discipline took care of. If the member cannot pay his light bill or water bill due to financial difficulties, until we take care of those needs through resources, any teaching that the nurse would do would be in vain. A person cannot focus on teaching for their health or anything else if their mind is on their current financial strain, not their medical condition. In this instance the nurse is playing the role of the nurse leader.
When a patient is in the hospital a nurse can also play the role of a nurse that is doing dressing changes, medication administration and other treatments. The nurse’s role in the interprofessional team that may consist of the doctor, physical therapist and dietician, would be more medically involved because maybe the patient is recuperating from heart surgery and requires a lot of care initially. The patient is on a special cardiac diet, which can also be explained by the treating nurse, however in this instance, the member is starting something new, so a consult from the dietician can help the patient understand the diet and the nurse can reinforce the teaching.
The nurse educator as part of the interdisciplinary team can be seen for example in a disease management setting. This type of setting also has multiple specialties that can follow the patient. In this instance the nurse educator is educating the member on how to empower themselves and learn about managing their chronic disease by learning about taking their medications, following a diet and exercise program, learning to check their blood sugar or blood pressure. The nurse educator measures the members learning based on return demonstration through development of a plan of care.
All three roles bring value to the scenario that they are in, because the nurse is the one that will be around the patient most of the time. In each role the nurses is responsible for all aspects of the patient’s care. In reading through the assigned readings for this week, I am able to see that although you have one nurse, that one nurse can play one of three roles depending on what scenario the nurse is in. Regardless of which role the nurse is playing, working on an interprofessional teams is a style of partnership that allows decision making to be collaborative (Sommerfeldt, 2013). It takes many people to work together in getting a patient discharged to his home.
References
Sommerfeldt, S. C. (2013, February 25 2013). Articulating Nursing in an Interpersonal World. Nurse Education in Practice, (13), 519. http://dx.doi.org/http://dx.doi.org/10.1016/j.nepr.2013.02.014
Follow Rosie Moore https://www.facebook.com/rosiesnursecorner/
Organizational Culture and Critical Thinking
In some managed care organizations, there are several factors that inhibit critical thinking skills to be utilized. Some of these factors are contract led and others are management style. Long term care programs are mandated by the state to follow a certain protocol on managing their cases for the members that are seen. The care part for the member is not an issue, however the reports and assessments that are required to be filled out, keep the case manager from adequately spending appropriate time with the member. If there is one item not completely filled out, the assessment will be returned by the state. The assessment is at times sent back late from the state, forcing the case manager to redo the entire assessment that can easily take two hours. This in turn causes a high turnover of staff because the demands on their time as salaried employees working 12 plus hours and 6-7 days per week are not what they want to do.
These company cultures do not lend themselves for new implementations for a better way to manage the staff and their time. The industry has seen some of the staff say that they have PTO (it should be paid time off) but at times they are still checking emails and phone messages for fear of getting behind, so one has to ask themselves are they on paid time off or pretend time off? One manager cannot implement changes in the entire company, but with their own team they can apply evidence based nursing and critical thinking skills to make a difference internally. 
Some ideas that a manager can work on with their team can be, discussing best practices for different aspects of the job. It seems that all team members and managers have to address emails, projects and reports, these will always interrupt the flow of the day. The team however, can control when they see their patients, make phone calls and when notes are entered in the system. When a manager is preparing to discuss the best practices, some things to consider can be based on the issues that the staff come up with ahead of time during the week or audits on their files. This can help the morale of the staff as well as their performance, decreasing the amount of turnover. (Marchionni & Ritchie, 2007)
In conclusion, every manager has their own style of managing. The best style of management is always going to be one that empowers employees to do their job based on examples and positive reinforcement. If all the employee ever hears is what they did wrong and never a word of praise, the employee will not strive after a while to grow and better themselves.
” A word aptly spoken is like apples of gold in settings of silver.” Proverbs 25:11
Written by Rosie Moore, RN, BSN , LNC
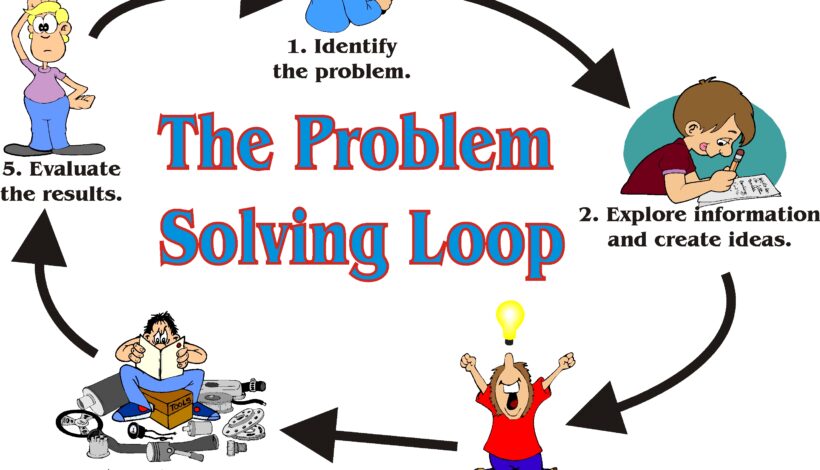
How Do You Use Your Critical Thinking Skills
Professionals use critical thinking and problem solving strategies daily in their work environment. Take for instance a health plan managing their member’s health, consisting of a staff of social workers, RN’s and LPN’s they will manage all kinds of medical conditions. The case manager is expected to apply critical thinking skills to each case and prioritize what that individual member needs. As an organization in healthcare they are to effectively encourage behavior change in members towards a healthier life that will avoid gaps in their healthcare treatment. The case manages are also required to achieve the business goals of the company by submitting state required forms timely to AHCA (Agency for Healthcare Administration). With each member that the case manager interacts with, they will be advising them of what care is covered under their plan, how they can best utilize the health plan to empower them to live a healthier lifestyle by complying with such things as attending their doctor’s appointments, taking their medications and reporting changes in their health, socioeconomic status or if their living arrangements are no longer safe for them.
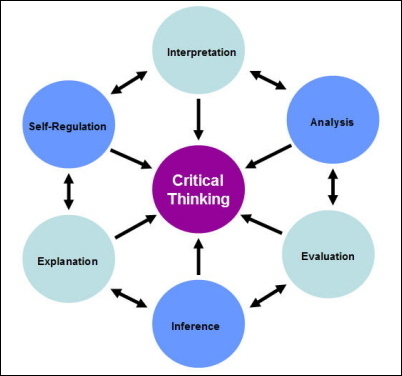
Every organization can improve the critical thinking of their staff, but the reality is that it is the staff member that needs to utilize their critical thinking skills to make that change. One thing I learned is that “To provide quality care in this environment, nurses need to develop critical thinking (CT) skills that will provide them with expertise in flexible, individualized, situation-specific problem-solving.” (Brunt, 2005, p.60) When I think of how some case managers use critical thinking skills, I become concerned. For example, I will share a story of a time that a social worker went out on a field visit with a nurse to a nursing home. The social worker had already informed the accompanying nurse that the member was non responsive and she will either sleep through the visit or have a blank stare. One of the first things the nurse noticed when she came in the room was that she had slipped in her hospital bed to the side. It is noted that the insurance company case managers do not do hands on care, so the social worker will have to let the nursing home staff know to readjust her.
Second the nurse accompanying the social worker noticed that she had a big bump on her forehead, she questioned the case manager but she did not know where that came from. The nurse quickly used her critical thinking skills to scan the situation and see that the member probably had slipped. During the nurse’s visit, she noticed that the member had too many pillows behind her back; she was a light weight and was slipping to the side about ready anytime to hit her head on the same spot with side rail. This led the nurse to believe that this was not the first time this had happened to this member. The nurse and social worker let the staff know on the way out of the member’s room.
However, in thinking about the list of 17 Dimensions of Critical Thinking in Nursing, a few critical thinking skills stand out in my mind for this situation that I was hearing about. When analyzing a situation, if the case manager is not a nurse who is used to doing head to toe assessments, would she have known that bump on her head was the result of the member falling sideways and hitting it on the side rail in the very same position that she was found in? If the social worker did not seek information from the nursing staff to ask about the bump on the member’s forehead and was only concerned for what is in the member’s chart, then she would not have the correct information to formulate a plan of care that will benefit that member. If the social worker could predict what would happen if the member continued sleeping sideways on the bed propped by pillows, then she would be using her critical thinking skills to avoid an incident. Transforming knowledge can only happen when you have a working knowledge on any subject. If you have not been taught how to do a physical assessment on someone, then you are not able to transfer what you were taught in a book to a real life situation that will require critical skills thinking to resolve a problem. (Rubenfeld & Scheffer, 2005, p. 2)
Rubenfeld, M. G., & Scheffer, B. K. (2005). Critical Thinking TACTICS for Nurses: Achieving the IOM Competencies (3rd ed.). [Vital Source BookShelf]. Retrieved from http://online.vitalsource.com/books/9781284059571
Written by Rosie Moore, RN, BSN, LNC